Abstract
Acute graft-vs-host disease (aGVHD) and cancer relapse remain the primary complications following an allogeneic hematopoietic stem cell transplantation (allo-HSCT) for malignant blood disorders. While post-transplant cyclophosphamide combined with standard GVHD prophylaxis has greatly reduced the overall prevalence and severity of aGVHD, relapse rates remain a concern. There is thus a need to identify the specific human T cell populations mediating GVHD vs GVL activity as a means to develop targeted therapeutics capable of controlling aGVHD without inhibiting GVL activity. In this study, we identify a novel human T cell population that develops after transplant that is predictive and sufficient for GVHD pathology.
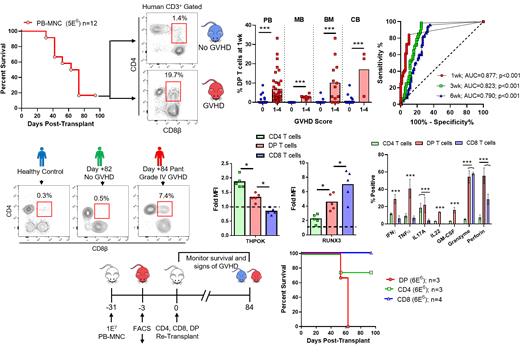
To determine the role of human T cell populations in aGVHD, we performed xenogeneic transplantation studies using primary human graft tissue from a variety of sources (peripheral blood, G-CSF mobilized peripheral blood, bone marrow and umbilical cord blood) in addition to collecting primary human aGVHD blood samples from our clinic. Using the LD50 dose of human graft tissue, we identified a novel mature CD4 +/CD8αβ + double positive (DP) T cell population that only developed after transplantation. The development of this population was further confirmed in aGVHD patients from our clinic. The presence of DP T cells, irrespective of graft source, was also predictive of lethal GVHD in as early as one week after xenogeneic transplantation.
To identify the origin of DP T cells, we transplanted isolated human CD4 or CD8 T cells into mice which showed that DP T cells only arise from the CD8 pool. Furthermore, re-transplantation of flow-sorted CD8 T cells from GVHD mice did not reveal a 2nd wave of DP T cell differentiation. This data, in addition to their highly proliferative state, suggests that DP T cells represent highly activated CD8 T cell clones. The ability of these CD8-derived DP T cells to gain CD4 expression coincides with their co-expression of both RUNX3 and THPOK, the master transcription factors of the CD8 and CD4 lineages respectively, that classically repress each other. Intracellular cytokine staining also revealed that DP T cells are the primary activated T cell population in xenogeneic GVHD, secreting both modulatory and cytotoxic cytokines (e.g. IFNγ, IL-17A, IL-22, perforin and granzyme). Ex vivo re-stimulation or re-transplantation of flow-sorted DP T cells showed that this T cell population is capable of dividing and expanding independent of CD4 and CD8 single positive T cells with the majority of the isolated DP T cells retaining their co-expression of CD4 and CD8.
Finally, transplantation of either isolated human peripheral blood CD4 or CD8 T cell populations were capable of causing lethal GVHD. Conversely, re-transplantation of flow-sorted DP, CD8 or CD4 T cells from GVHD mice revealed that DP and CD4 T cells are sufficient to mediate GVHD pathology but re-transplanted CD8 T cell are not. This correlates with the absence of DP T cell differentiation in that re-transplanted CD8 population. The differentiation of DP T cells from chronically activated CD8 T cells represents a novel mechanism of GVHD pathology not previously described. The presence of DP T cells in other chronic inflammatory human diseases also suggests a broader pathology mediated by DP T cells. Further understanding of DP T cell differentiation and pathology may lead to targeted prophylaxis and/or treatment regimens for aGVHD and other human chronic inflammatory diseases.
Capitini: Nektar Therapeutics: Honoraria; Novartis: Honoraria.